interferon alfa 2b

interferon alfa 2b
CLINICAL USE
Intron A:Chronic hepatitis B —Chronic hepatitis C —Hairy cell leukaemia —Multiple myeloma —Carcinoid tumour —Chronic myelogenous leukaemia —Follicular lymphoma —Malignant melanoma —DOSE IN NORMAL RENAL FUNCTION
Chronic hepatitis B: 5–10 million IU 3 times a weekChronic hepatitis C: 3 million IU 3 times a weekHairy cell leukaemia: 2 million IU/m 2 3 times a weekMultiple myeloma: 3 million IU/m 2 3 times a weekCarcinoid tumour: 3–9 million IU/m 2 3 times a weekChronic myelogenous leukaemia: 4–5 million IU/m2 dailyFollicular lymphoma: 5 million IU 3 times a weekMalignant melanoma: 20 million IU/m 2 (IV infusion
) daily for 5 days, decreasing to 10 million IU/m2 (SC) 3 times a weekPHARMACOKINETICS
DOSE IN RENAL IMPAIRMENT
GFR (mL/MIN)
DOSE IN PATIENTS UNDERGOING RENAL REPLACEMENT THERAPIES
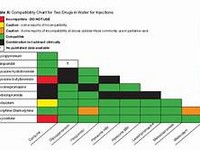
IMPORTANT DRUG INTERACTIONS
Potentially hazardous interactions with other drugsImmunosuppressants, e.g. ciclosporin, tacrolimus, sirolimus may have an antagonistic effectAdministration of interferon in combination with other chemotherapeutic agents, e.g. cytarabine, cyclophosphamide, doxorubicin, teniposide may lead to increased risk of severe toxicityADMINISTRATION
Reconstition
–Route
IM, SC, IVRate of Administration
20 minutesComments
Add to sodium chloride 0.9%OTHER INFORMATION
Interferon up-regulates the cell surface presentation of class II histocompatibility antigens, which raises the possibility of drug-induced allograft rejection. There are numerous clinical reports of allograft rejection, acute renal failure and graft loss after interferon therapy. Hence extreme care should be exercised in the use of interferon after renal transplantationInterferon is metabolised primarily in the kidney. It is excreted in the urine, but is reabsorbed by the tubules where it undergoes lysosomal degradation. In patients undergoing haemodialysis, the interferon molecule may accumulate as it is too large to be dialysed and will not undergo renal degradation. Hence, the dose may need to be adjusted
See how to identify renal failure stages according to GFR calculation
See how to diagnose irreversible renal disease
Home